How Increasing Access to Digital Services Can Destigmatize Mental Health Among Minorities
By Sydney Charles, Jeremy Lindenfeld, Charisma Madarang, Anaja Smith, and Wesley Stenzel
For millions of people of color, America’s ongoing racial reckoning – from police brutality against Black Americans, anti-Asian violence, and immigrant children in cages to a virus that disproportionately impacts communities of color – is a weight BIPOC communities never asked to bear but cannot escape. This confluence of crises has led to an increased need for mental health services among many minority communities, and digital advances have made these services more accessible than ever before.
Dr. Lorra Garey, a researcher who specializes in mental health at the University of Houston, says she’s seen an increase in anxiety and depression since the pandemic began. “People who identify as BIPOC are experiencing prolonged negative mental health effects from the pandemic that will likely continue for some time,” she says.
The internet offers a glimmer of hope: a massive boom of virtual services transformed the landscape of mental health treatment, providing unprecedented access to historically underserved communities. In 2020, the American Psychological Association estimated that there were over 10,000 mental health apps available to consumers. Dr. Quade French, a clinical psychologist at USC, says, “The transition to online or app-based teletherapy has increased accessibility across the board.”
Mental health apps and teletherapy providers are racing to adapt their platforms to be more inclusive, accessible and mindful of the unique experiences of BIPOC during this time. This reactive evolution prompted many apps to offer more free services in an effort to make them more marketable.
“There is this real anxiety that wasn't there before.”
— Tiffany Sun
The popular wellness app Happify redirected its focus after the Atlanta spa shootings, working to create a custom series of wellness exercises for the AAPI community. “It was in the news, people on staff were experiencing it themselves, we were even hearing it from clients, from users: there is this real anxiety that wasn't there before,” says Tiffany Sun, Happify’s Chief Content Officer. Other apps have taken a similar approach. Sanvello, a teletherapy and coaching app, created a space where BIPOC users could come together to discuss the stress and anxiety of the pandemic.
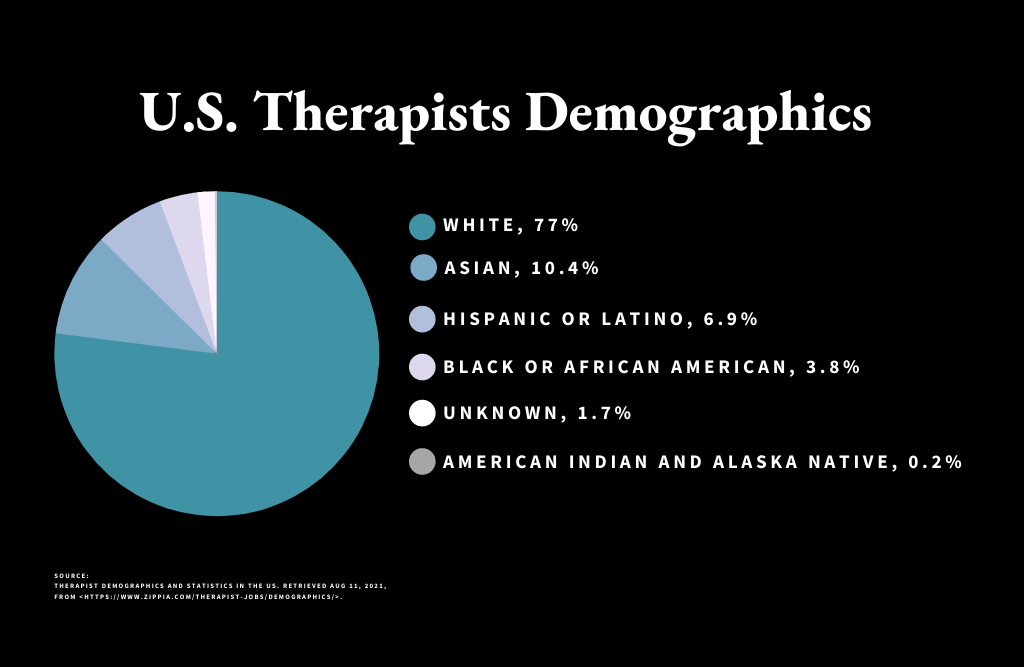

Still, French explains that structural issues make mental health services unwelcoming to members of BIPOC communities as there is a “systemic lack of access provided to Black and Indigenous persons of color,” and that health care systems in general “weren't designed to support people from marginalized communities.” Career demographics database Zippia reports that 77 percent of therapists in the U.S. are white and Black therapists make up just 3.8 percent, despite the Census Bureau reporting 13 percent of people in the U.S. identifying as Black. This overwhelming whiteness of American therapists means that many individuals of color cannot rely on most counselors to understand their experiences. BIPOC are often expected to educate their therapists about social issues, which is a symptom of a broader dilemma: the constant assumption that BIPOC must bear the emotional burden of white ignorance.

Kevin Palmer
Los Angeles resident Kevin Palmer understands this dilemma all too well. Soon after George Floyd’s death, Palmer received a call from a white coworker. When he picked up, she was sobbing.
“I’m sorry this is happening right now,” she said through tears. “I know you’re sensitive about these things.” It was a sentiment she would repeat throughout the call, which felt more like a confession than an apology to Palmer. Hers were tears he did not want to hear, another show of white guilt that expected absolution in return.
None of it surprised him. Palmer, who works in an industry dominated by white men, has spent much of his career dealing with microaggressions and racism in the workplace. Once, during a meeting in front of hundreds of Mexican factory workers, his director announced that his company was proud to be “male, pale, and stale.”
The relentless media exposure to racial traumas, pandemic isolation, and the initial silence from his company – followed by a “generic” email of solidarity with its Black employees – took such a profound toll on Palmer’s headspace that he began to seek professional guidance.
“It was one of those things where it was extremely difficult for me to navigate my own thought processes and still want to work and still want to be able to be a good salesman. To still want to provide value to a company that didn't seem like it was really valuing me,” he says.
Kevin Palmer on his teletherapy experience.
Palmer saw therapy as a necessary step to self-development. “Now is as good a time as any,” he says. “I had no excuse not to.”
His search led him to finding a therapist, available via teletherapy, within his own community – a Black man living in Los Angeles who was able to empathize and listen from a place of shared understanding. “It was like it was understood and he got it,” Palmer says. Together with his therapist, Palmer was able to process and reframe stressful situations with intention.

Adaeze Oduma
For Adaeze Oduma, finding a therapist who understood her identity was key. “I want somebody who looks like me,” Oduma says. “In my case, it’s not just somebody who is Black, somebody who is also queer, somebody who is trans or at least has very deep understanding about those things.”
She had seen therapists prior to 2020, but the industry’s pandemic-induced digital shift made it possible for her to get support from virtually anywhere. Additionally, digital services allowed her to try several different therapists before finding the one best tailored to her needs.
A poem by Adaeze Oduma.
Oduma, who identifies as non-binary and welcomes all pronouns, is the child of Nigerian immigrants whose strict Catholicism impeded her wellness. The family’s attitude toward treatment was stern. “If your kid has to go to therapy, you fucked up royally in some way,” Oduma says. She says faith inclined them to “pray away” problems rather than seek external help. It took the revelation of a years-prior suicide attempt to finally convince Oduma’s parents that counseling was necessary – and even then, Oduma suspects that Catholic guilt informed her parents’ change of heart.
The stigma of mental health for communities of color has long been compounded by underlying racism, a lack of access to services and a belief that therapy is for people who cannot handle challenges.
William Behvandi, a second-generation Iranian American, acknowledges that stigma and toxic masculinity play a detrimental role in many Iranian men’s mental health. “I feel a stereotypical ‘bottle it up, go to work, deal with your problems’ mentality just doesn't work,” says Behvandi.

William Behvandi
Behvandi sought the help of a therapist to help him manage his panic attacks. Luckily, he had the emotional and financial support of his parents, which he pointed out is a deviation from the Iranian American norm. “My parents are the most understanding Iranians I know in their circles,” he says. Through the BetterHelp app, Behvandi connected with Dr. David Shapiro, a specialist in anxiety and depression. They met in weekly half-hour sessions to equip Behvandi with techniques to mitigate his symptoms. Within four weeks of treatment, he went from experiencing a panic attack every other day to just once a week. Within two months, the attacks were completely gone.
Digital mental health services are far from perfect, however. Online platforms don’t completely fix the existing financial burden inherent to the industry. While many mental health apps do provide their introductory services for free, often there is a paywall for its more high quality services and connecting with a real, human therapist is often not covered by insurance. “I found somebody who hit every single one of my boxes, I was like, ‘This is impossible, they’re a unicorn!’ – but they didn’t accept my insurance,” Oduma says. Behvandi was only able to afford BetterHelp with assistance from his parents. “It definitely favors people with more income right now because it's really expensive,” Behvandi says. “In lower income neighborhoods, I can't even imagine how they go out to try to get help.”
Audio Stories

William Behvandi on discovering teletherapy

Kevin Palmer on a poor therapy experience

Adaeze Oduma on convincing her parents she needed help
While there is more work to be done, digital advances and growing discussions about prioritizing mental health among BIPOC offers a promising look at the future: An open dialogue where vulnerabilities are not only seen as strength, but a place to grow from.
“I took it upon myself and essentially said that this would ultimately be better for my relationships, social relationships, romantic relationships, future relationships, relationships with my family and future kids,” Palmer says. “I said that was an investment I'm willing to take, and that's for me.”
Mental health resources for BIPOC
Click the boxes to explore resources!
Inclusive Therapists
Open Path Collective
National Queer & Trans Therapists of Color Network
South Asian Therapists
Latinx Therapy
Black Emotional and Mental Health Collective
Ayana Therapy
National Alliance of Mental Health - BIPOC/AAPI Mental Health Resources
Asian Mental Health Project - Hotlines & Outreach Template
Asian Mental Health Collective
Therapy for Black Girls
Therapy for Black Men
