Charles Johnson IV paces the empty waiting room at Cedars-Sinai Medical Center, awaiting word about his wife, Kira.
Earlier in the day, joyful families waited with balloons to welcome newborn babies into the world. The Johnsons had been one of those families, celebrating the arrival of their second son, Langston.
But now it's the middle of the night. The room is quiet. Johnson waits alone. It's been much longer than the 15 minutes the doctor, who only hours earlier had delivered their son by cesarean section, promised it would take to stop the internal bleeding.
After midnight, two doctors and a trauma surgeon walk into the room to deliver life-changing news. "When they opened her up, there were three liters of blood in her abdomen," Johnson said. "Her heart stopped immediately." His wife, Kira Dixon Johnson, 39, died on the operating table.
Every year, about 700 women die nationwide due to pregnancy-related causes, according to the Centers for Disease Control and Prevention. Another 50,000 women experience severe complications. Black women, who are three to four times more likely to die than white women, are at the highest risk. A report by The American College of Obstetrics and Gynecologists suggests implicit bias on the part of health care providers may contribute to racial health disparities.
For Johnson, coming to terms with the role race may have played in his wife's death is painful. "The fact that all of these things could've gone wrong because of the color of her skin, I hadn't even begun to a process that," said Johnson. "But I do feel in my heart that if she had been Caucasian, maybe she would have been back to surgery a couple of hours earlier and that might've made the difference."
The same race disparity exists in California, the state with the lowest overall maternal mortality. Black women remain three to four times more likely to have a fatal outcome, the California Maternal Quality Care Collaborative found.
Researchers and medical practitioners seeking the causes of health disparities in obstetrics and gynecology, point to genetics, health behaviors, and socioeconomic status as contributing factors. Another problem that continues to gain attention from public health experts, politicians, and the media, is implicit bias by health care providers and the growing perception that black women are often ignored by doctors and hospital staff. "Health equity for black women can only happen if we recognize and address persistent biases in our health system," says 2020 presidential candidate Kamala Harris, in an email. "That's why I've introduced the Maternal CARE Act to fund implicit bias trainings for health professionals."

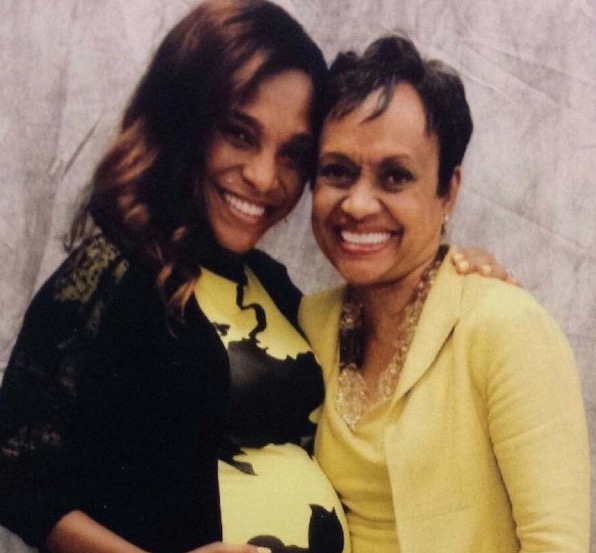
Kira Dixon Johnson
Since his wife's death, Johnson founded the non-profit organization, 4Kira4Moms, with the mission of improving maternal healthcare policies nationwide. In December 2018, Johnson played a key role in getting the Preventing Maternal Deaths Act signed into law. The law provides $12 million in federal funding for five years to establish maternal mortality review committees in all 50 states. These committees will be responsible for investigating each maternal death and reporting their findings to the CDC in a standardized format. "I'm hopeful," says Johnson. "There's a lot of work that needs to be done, but this is an important first step."
4Kira4Moms is a member of the March for Moms Alliance, a coalition of about 40 organizations, including The American College of Nurse-Midwives, and Doulas of North America who are working to reduce maternal mortality. "Because it is a complex issue, one of the challenges is there are a lot of people that are working very hard, but the approaches and the solutions have been siloed," says Johnson.
Across the country, black doulas are working to bridge the health gap by taking care of the black moms in their community. A doula is someone who is trained to provide continuous emotional, informational, and non-medical, physical support to moms before, during, and after pregnancy. A report published by The American College of Obstetrics and Gynecology suggests that continuous one-to-one emotional support provided by support personnel, such as a doula, can improve outcomes for women in labor. The March of Dimes suggests access to doula care is one tool that can improve birth outcomes and reduce the higher rates of maternal morbidity and mortality among women of color in the United States.
Black Midwives and Doulas Embrace a Community Approach to Maternal Care
In Johnson's hometown of Atlanta, Georgia — the state with the highest maternal mortality rate and where 79 counties do not have an obstetrician or gynecologist — a midwifery practice is taking a different approach to maternal care.
Marsha Ford, runs OB/GYN and Midwife Associates in East Point, where 90 percent of her patients are black. Ford, who has been a certified nurse midwife for 26 years, encourages all of her moms to get a doula. "You need that village." Ford tells her patients. On any day of the week, doulas can be found in the waiting area at Ford's practice. "Ms. Ford," as the doulas call her, embraces an open-door policy and encourages doulas to come in to market their services and teach childbirth education classes.

Left to Right: Corrinna Edwards, Marsha Ford, and UmmSalaamah Abdullah holding a quilt that has custom patches to honor women who died during childbirth. Kira's patch (center) features a blue bird.
"Most practices will have cards for doulas they might recommend or work with, but no one's really pushing it," says Corrinna Edwards, a doula and midwife who often partners with Ford's practice. The open-door policy helps Ford get to know the doulas in the community and make more personalized recommendations to her clients. "Then I can say, 'I know somebody that could be good for you,'" Ford says. "I think they accept it more than just giving them a piece of paper."
White women pioneered the doula profession, but black communities have a long history of women supporting other women giving birth. "There were no doulas," said Edwards. "We did it. It was your mother, your grandmother or your sister, your auntie, that type of thing." An evidence-based study from the Cochrane Library, a database for systematic reviews in health care, revealed that "Modern obstetric care frequently means women are required to experience institutional routines. These may have adverse effects on the quality, outcomes and experience of care during labor and childbirth." As the birthing process became more medicalized, the importance of having someone in the room for the sole purpose of supporting the mother was lost.
This year, Johnson plans to focus his efforts in Georgia. "Not only are we 50th in maternal mortality, we're 49th in infant mortality," said Johnson. "So stuff is bad here."
Medical Improvements Don't Reduce Race Disparities
In California, where moms have the best chances of survival, Johnson learned the news of his wife's death from two residents and a trauma surgeon he had never seen before. Johnson was in a state of disbelief, and could not understand why Dr. Arjang Naim, the doctor who performed the surgery, and who had delivered their son hours before, relegated the task to others. "He never even came out to give us the news that she died," he said.
After Kira died, Johnson remained at the hospital for a couple days with his newborn son, changing diapers and doing feedings. He still heard nothing from the doctor. It would be many days before Johnson could begin to make sense of his life without Kira. The couple started several businesses together and had relocated to Los Angeles to be executive producers of "The Verdict With Judge Hatchett." Johnson's mother, Glenda Hatchett, is the star of the TV court show.
Two days later, Dr. Naim met with Johnson, with his mother, and in-laws also in the room. "When we ask him what happened, he starts saying stuff like, maybe she had a heart problem and goes through a litany of excuses," says Johnson, who thought the doctor was evasive and insensitive.
"Finally, I stopped and said, 'Let me ask you a question. What would you have done differently if this was your wife?'" recalls Johnson. "And I still can see it as clear as day, the look that he had on his face. He was just perplexed. So I ask him a second time and he says, 'Well, what do you mean?'"
Johnson asks the doctor a third time what he would have done differently if Kira had been his wife.
"He just sits there with this bewildered look on his face and his response to me was, 'Do you mean as a doctor or as a husband?'" At this point, Johnson asks the doctor to leave. To Johnson, Dr. Naim failed to see his wife as a valuable human being.
Dr. Naim was placed on probation for four years by the Medical Board of California. Johnson sued the hospital and doctor, alleging wrongful death. No trial date has been set.
Using the medical records from Cedars-Sinai Medical Center, the lawsuit includes a timeline of the hours leading up to Kira's death — chronicling the number of times multiple doctors and nurses came in to run blood tests and monitor Kira's condition. At 6:44 p.m. a CT scan of Kira's abdomen and pelvis was ordered "stat" — for surgical emergency. At 10:44 p.m. those scans had still not been done and records indicate that they were never performed, according to the wrongful death suit.
"I really have no idea how many times I talked to different nurses, how many times I talked to different doctors, how many times I ask questions the whole time getting the runaround," says Johnson.
Three years after his wife's death, Johnson continues to work on legislation that would establish a fundamental standard of care for postpartum health. "There is too much arbitrary decision-making when women are in a crisis," says Johnson. "What I'm going to push for is a real mandate tied to Medicare and Medicaid reimbursement. If hospitals aren't meeting the standard, they don't get their money."
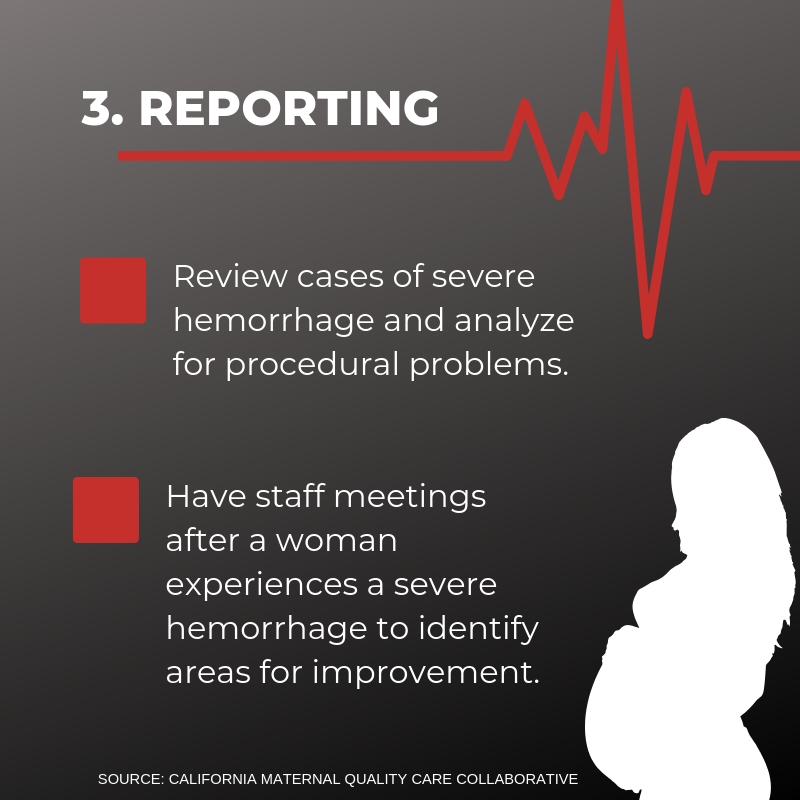
In California, the Maternal Quality Care Collaborative analyzed data gathered from death certificates and medical reports and created toolkits to address problems identified in their reviews. The early years of research found that obstetric hemorrhage, like the one that killed Kira Johnson, was one of the most preventable causes of maternal mortality. The Obstetric Hemorrhage Toolkit, released in 2009, had been adopted by 92 percent of California hospitals by 2016, according to the Collaborative. "If you think about hemorrhage, it's very much about having the right sort of processes and procedures in place," said Cathie Markow, administrative director. "And being able to respond to a hemorrhage very quickly."
Johnson says he didn't know Cedars-Sinai Medical Center had access to the hemorrhage carts until after his wife's death. "The question I have is why didn't anybody turn to those resources in Kira's case? Why did they let her suffer and hemorrhage internally when they knew she was bleeding for 10 hours?" asks Johnson. "When those solutions are suggestions and not mandates, women, like Kira, slip through the cracks." Cedars-Sinai Medical Center would not comment on specifics relating to Kira's case, but emailed a statement:
"Charles S. Johnson IV is demonstrating important leadership in raising awareness of preventable maternal deaths. Cedars-Sinai faculty members support efforts to improve care and prevent maternal deaths, and are actively involved in community, state and federal initiatives to safeguard the lives of mothers and their babies. We can share that Cedars-Sinai thoroughly investigates any situation where there are concerns about a patient's medical care."
In the months and weeks leading up to the birth, doulas are there to educate women on what to expect during the childbirth process by answering questions, providing resources for women to learn about different birth options, and teaching different coping and pain relief techniques. "Doulas help families navigate the system," said Durdin. However, one of the main responsibilities of a doula is to support the laboring woman during the birth.
"A lot of times women are looking for a birth worker that looks like them. Coming from a similar culture to the family that you're serving can be a huge benefit." said Durdin. "It kind of allows them to be like, OK, I know we're good, we don't have to explain what being a black person in America is like. That holds a lot of weight."
Click image to enlarge

Miller gave birth to a baby boy on Jan. 23. Both mother and baby are healthy and encountered no serious complications during the delivery, but Miller recalls feeling exasperated by one of her care providers, who was a white woman.
"I had a situation with this nurse," said Miller. "I was in a lot of pain, the contractions were coming back-to-back and this nurse kept giving me instructions like 'lift up' or 'I have to put this here' and I was just like give me a minute!"
Miller grew frustrated with her nurse's lack of patience, but said that her doula helped restore the calm. "Christian would actually be really patient with me and when I would have a contraction she would push on my lower back and she would help me." Beckley said the nurse gave good care, but was pushy. "What I think the nurse got wrong is the consent part, asking if it is OK if I touch you."
Research shows that lack of continuous support during childbirth leads to concerns that the experience of labor and birth may have become dehumanized. A survey of black mothers in California found communication during labor to be a problem. Almost one-third of black mothers reported that they did not feel the delivery room staff encouraged them to make decisions about their birth progression, whereas only 20 percent of white mothers reported feeling the same lack of encouragement.
"When the doula comes, we are like the cheerleaders for the football team. We're also the fans in the stands. We're the waterboy. We're the team manager," said Beckley. "We use words of affirmation to tell you, 'You can do this, believe in your body, your body was made to do this.' We're your biggest fan."
Johnson is Respectfully Demanding Change
Outside of the Georgia State Capitol, Johnson stares up at the golden dome that sits atop the historic building while his two sons Charles V, 4, and Langston, 3, play on the lawn. He's here to receive a resolution from the state legislature for his advocacy and attention to the issue of maternal health. As the guest of honor, Johnson is given the floor to address state legislators. "I'm respectfully demanding that the state of Georgia send a loud, definitive message to this country that mothers and babies matter."
While Johnson is looking up at the Capitol building, his youngest son suddenly stops playing, runs over to him and hugs his legs. Langston begins pointing to the sky, recalls Johnson. "I squat down and hug him and he puts his head on my chest right where I have this pin of Kira," said Johnson. "And he starts patting the pin and kissing it."
Since deciding to go public with Kira's story on Mother's Day two years ago, Johnson is proud of what he accomplished. But he shares the credit. "It's really Kira," he said. "When people see her, when they hear our story, it's really Kira's spirit touching people she's never met in amazing ways."
Johnson says his activism sets a positive example for his two young sons. What keeps Johnson up at night is knowing one day he must tell his sons how their mother died. He hopes his work ensuring other mothers get to go home with their babies will make them proud. For Johnson, the motivation is simple. "Every day, it's wake up, make mommy proud, repeat."